Evalynn Linnea Olson
11/26/1959 – 11/15/2021
As many already know, it is with heavy heart that we share news of Linnea’s passing.
She was able to pass away at home, her adult children and family members were with her, and her clinicians and hospice team provided the full care and support she needed. It was very important to Linnea to be able to make an anatomical donation to the Mass General Cancer Center lung cancer research lab instrumental in her care. Together, her family and friends were able to help achieve all of her final wishes.
On Friday, December 3rd, Linnea’s family and friends will host a reception in her honor. The event will be held 6PM – 9PM EST at Maria’s Restaurant, 81 Essex Street, Haverhill, MA. For more information about this event, please visit: https://www.mykeeper.com/event/celebration-of-life-evalynn-linnea-olson/
If you cannot participate in person, join us for a Livestream at Linnea’s celebration of life in which we will reflect on her youth, her mission as an advocate for the lung cancer community, and her impact as a visual artist.
Link to the livestream event: https://fb.me/e/2Rg4j4dTe
Amesbury, MA – Evalynn Linnea Olson, known to all as “Linnea”, died at the age of 61 on Monday, November 15, 2021. She was a mother, loved by family and friends for her vast artistic mind and warrior spirit, as well as a fierce advocate and blogger for the cancer community while living with lung cancer for 17 years. Linnea is survived by her three wonderful children, Jemesii Delande and Peter Duff of the greater Boston area and August Kaan of Toledo, OH.
Linnea was born on November 26, 1959, in Ann Arbor, MI, the eldest child of Dr. Hilding Gunnar “Ollie” Olson and Evalynn (Pier) Olson Betzing Goodman. She shared her life with her extended family, including her step-mother Carolyn Olson Kersten of San Angelo, TX, her step-father James Goodman of St. George, UT, and her deceased step-father Richard Betzing of Fort Collins, CO. She enjoyed an active childhood with her six brothers and sisters: John Olson and his wife Amanda (Fort Collins, CO); Kristin “Bink” Owsley and her husband Greg (Fort Collins, CO); Laura Pastor and her husband Andy (Austin, TX); Diana Galvin and her husband Bobby (Temple, TX); Daniel Olson (Anchorage, AK); and Rosalie Olson and her husband Brian Dougherty (Boulder, CO). She is also survived by her nine beloved nieces and nephews, including Shannon Olson Payne; Mesa and Zola Owsley; Jacquelynne Amaro; Max, Eli and Hale Pastor; Magnus and Alma Dougherty; her grandniece Jordynne Amaro and grandnephew Iverson Mentel. Being with her family brought Linnea tremendous joy and fueled her incorrigible zest for life.
Linnea graduated from Poudre High School in Fort Collins, CO in 1977. She pursued her passion for oil painting and received a bachelor’s degree in Art, Painting Concentration from Colorado State University in 1981. Following this, she lived in Fort Collins and later the San Francisco Bay Area where she began raising her children and working at the Palo Alto Public Library. In 1996, Linnea and family moved to Ipswich, MA, later residing in Meredith and Amherst, NH, and Lowell, Haverhill and Amesbury, MA. As a lifelong artist, Linnea had an incredible eye for finding beauty in the ordinary – which she captured in her paintings, curated collections and nature photography. She found inspiration in beaches and sidewalks, rivers and train tracks- constantly in a state of creation.
In 2001, despite her active, healthy lifestyle, Linnea began experiencing challenges with her health, progressing to a long bout with pneumonia. As an otherwise healthy, young, non-smoking female, accurate diagnosis was elusive. After several years of medical evaluations, her life was changed when she was diagnosed with stage 1B lung cancer. Her youngest child was still in elementary school. Determined to be present for her family, she pursued clinical care at Massachusetts General Hospital (MGH), where she was followed by the oncology teams of Douglas J. Mathisen, MD, Thomas J. Lynch, Jr., MD, Alice T. Shaw, MD and Jessica J. Lin, MD.
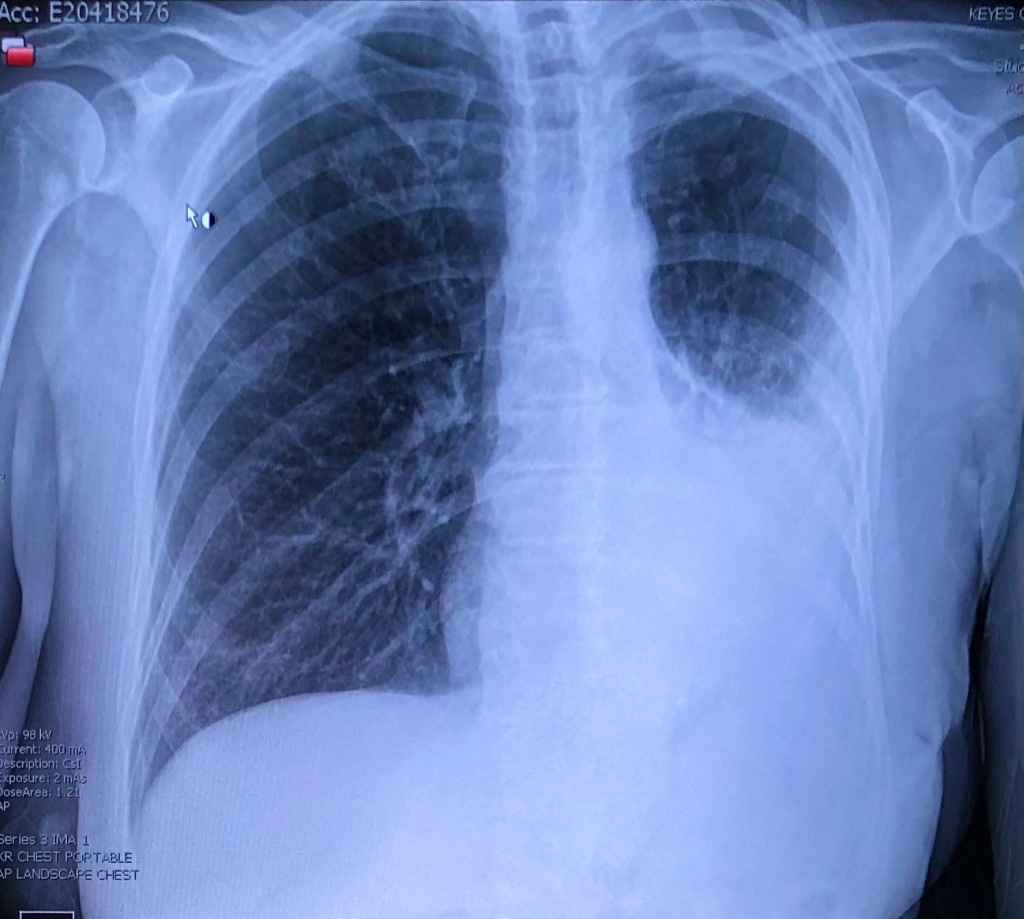
Due to the advanced nature of her cancer, Linnea found herself as a patient at the forefront of cancer treatment and research. With deep belief in scientific research and a voracious need for more time, over the space of 17 years she was a participant in six clinical trials, which served as landmark studies that changed the course of lung cancer targeted therapy the world over. Her body responded well to the novel therapeutics, to the extent that medical imaging scans of her lungs, before and after treatment, are still shown on display at the Paul S. Russell Museum of Medical History and Innovation at MGH.
In 2005, Linnea’s natural inclination to connect with others, along with her poetic yet precise way with words, led her to create a blog entitled: “life and breath: outliving lung cancer – for the terminally optimistic” (outlivinglungcancer.com). Her blog soon became a resource for more than 4,000 followers, from patients and caregivers to physicians and biomedical researchers. Her well-informed and bravely candid writing shared essential resources and medical knowledge, while also giving voice to what it is often like for patients living with cancer. With honesty and humor, her writing created a community which stands as a testament to who she was. Linnea had a curiosity for life and learning, a talent for teaching, and an unyielding desire to share her unbiased, truthful observations of the world around her.
Always a strong patient advocate, Linnea’s work touched the lives of people around the world. She presented at numerous forums, including Harvard Medical School, TED Talks, industry presentations and international conferences. In 2016, Linnea was awarded LUNGevity’s Survivor Face of Hope award for her tireless work on behalf of fellow patients and served on the External Advisory Board of their committee “Patient FoRCe.” She was also honored as the 2020 Recipient of the LUNGevity Annual Fan Award. In 2019, she served on a group panel at the World Conference on Lung Cancer in Barcelona, Spain to address best ways to support patients and clinicians in their search for clues to combat lung cancer. She joined the board of trustees of the Israel Cancer Research Fund (ICRF.org) shortly thereafter. She was a 2020 recipient of A Fresh Chapter foundation grant to visit with fellow cancer patients in Peru. Additionally, she was on a Hackathon in 2021 to promote efforts to find new drug therapies.
Linnea identified equally as both advocate and artist. Between 2012 and 2019 she lived at the Western Avenue Studio and Lofts – an artist’s community in Lowell, MA. Linnea was well known to all as a friend, an informal counselor and generous spirit. While she spoke of herself as a painter, Linnea’s artistic identity was as often defined by an insatiable desire to collect and curate. Linnea packed her studio with fascinating collections of shells, sea glass, bell jars, books, antique doll heads, globes, vintage clothing, rusted bits of metal, pieces of discarded paper and wood and an impressive array of other interesting things she found on her frequent walks, thrift store trips and eBay scourings. She had an incredible eye as curator, turning seemingly unwanted, discarded items into stunning collections. 2018, her last exhibition, Found, at the Linda Hummel-Shea ArtSpace Gallery of Northern Essex Community College presented dozens of assemblages — combinations of found objects that together create new poetic meanings. These works embodied Linnea’s drive to find deeper meaning in her life through her art and collections- and her deep love for the often overlooked or forgotten.
One of Linnea’s most sacred daily routines was a long, wandering walk which became even more important after adopting her energetic Shiba Inu, Kumo. Linnea often documented her walking observations in a series of Facebook posts she called “Notes from the Field.” Reading them offered a glimpse into Linnea’s heart and mind. On March 21, 2021, Linnea wrote:
• Tree trunk, knot like a navel.
• Sun wraps the back of my head.
• Plastic bag caught on a branch; pale ghost.
• Wind chimes sounding like summer.
• Sunday morning paper.
Her friends will carry Linnea’s inspiration in every walk while she reminds them to keep their eyes open to the beauty of the world around them and to remain always curious.
Linnea’s family and friends offer their deepest thanks to the incredible team of providers at the Mass General Cancer Center. Their intellect, kindness and devotion to patient care is exemplary. Gratitude for the kindness of friends who helped Linnea throughout her journey. Sleepovers, rides, dinners, unanticipated flower bouquets, dog walking and assistance in many forms enabled Linnea to live fully and vibrantly. Know that each act of kindness meant the world to her.
A celebration of her extraordinary life will be held on Friday, December 3 from 6PM – 9PM at Maria’s Restaurant – Galleria Banquet Room, 85 Essex Street, Haverhill, MA. For more information, please link to: rememberinglinnea.com. Out of an abundance of caution for family and fellow guests, attendees must be fully vaccinated against COVID-19 and wear masks. Donations in Linnea’s honor can be made to LUNGstrong.org (which will be directed to MGH lung cancer research), LUNGevity.org or ICRF.org.